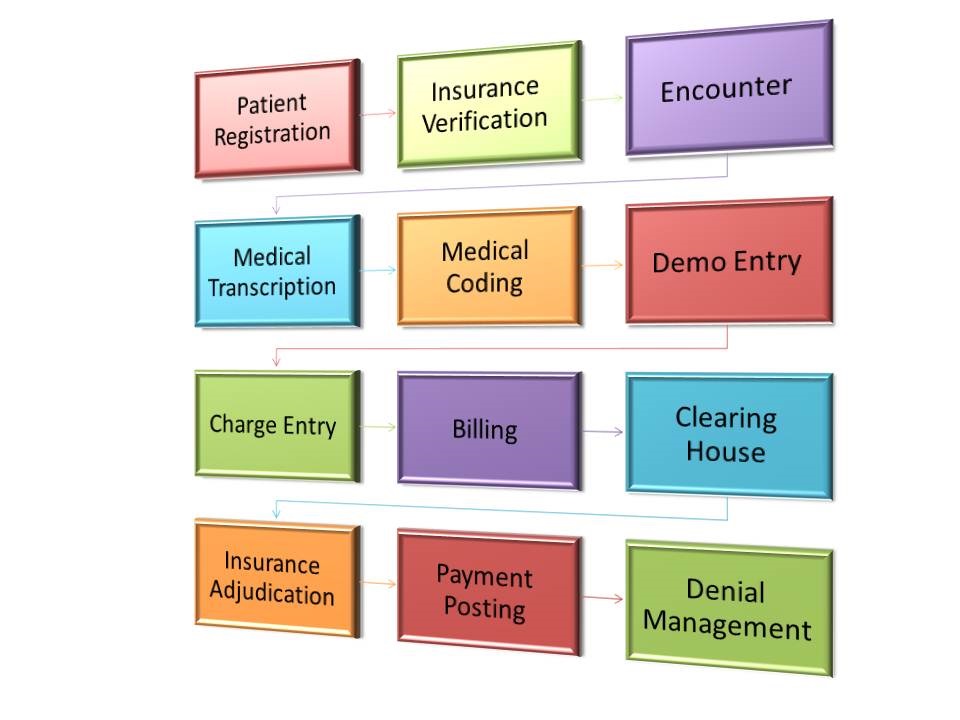
Patient Registration/Demographics entry
Initial process of Medical billing is Patient registration, which includes the entry of basic information and demographic information of the pateint into the medical billing software provided by the Provider office. An new account would be created for each patient to keep track of the complete Medical and transaction history of a patient.
Insurance Eligibility verification
Eligibility verification is the most important and the first step in the medical billing process. Research confirms that most of the claims are denied or delayed due to inadequate or incorrect coverage information provided by the patients during visits and current coverage information not updated by the office / hospital staff. This lack of or improper insurance eligibility verification directly impacts the reimbursements.
Medical Coding
All healthcare entities are looking forward to the next radical change, which is the ICD-10 medical coding implementation. This transition to the ICD-10 code sets is expected by Oct, 2015 and Facilities, clearing houses, Payers and medical coding companies have already started preparing for the change. This transition to the ICD-10 codes is set to bring about efficiencies in improving patient care, increasing physician billing accuracy, enhancing clinical performance and several other benefits that the ICD-10 medical coding transition is slated to augment in the first few months of its implementation.
Charge Entry Services
Charge entry is one of the key areas in medical billing. In the medical billing charge entry process, created patient accounts are assigned with the appropriate $ value as per the coding and appropriate fee schedule. The charges entered will determine the reimbursements for physician’s service. Therefore, care should be taken to avoid any charge entry errors which may lead to denial of the claims. Moreover, good co-ordination between the coding and the charge entry team will produce enhanced results.
EDI Setup
Operomed can do a complete EDI set-up for new practices or practices moving from paper based claims to electronic forms. The process includes setting up the user and database on the EDI (Clearing House) website, testing with sample batches to ensure that the 837 and 835 are processed correctly and integrating the EDI with the Billing system for ‘one touch’ transmission of claim batches. Other aspects that can be set-up are 276/277 (Claim Status) and 270/271 (Eligibility and Benefits verification).
Payment Posting
The payments in lieu of claims, which are received from the Payer and Patients, are posted in the medical billing system of the client to reconcile the claim. We also does electronic payment posting in to the medical billing software and handles the exceptions (fallouts) manually to make sure no payment is missed. The posted ERAs are stored either in the billing system or a Document Management system (DMS) for future reference.
Insurance Payment Posting
All payers either send an EOB (explanation of benefits) or ERA (electronic remittance advice) towards the payment of a claim. The medical billing staff posts these payments immediately into the respective patient accounts, against that particular claim to reconcile them. The payment posting is handled according to client-specific rules that would indicate the cut-off levels to take adjustments, write-offs, refund rules etc.
When the client’s office delays in either depositing the Payer checks or sending the ERAs and EOBs for posting, then a negative balance prevails for that claim, which is a false representation of the actual scenario. This false representation would show an inflated AR, resulting in the Physicians not knowing exactly how much revenue is due to them.
Patient Cash Posting
There could be several reasons why the patient needs to pay a part of the expenses including co-pays, deductible and non-covered services. If the amount due from the patients is very minimal, the Provider can set a mandate for taking write-offs. If the amount is quite large, then it should be collected from the patients either prior to or after rendering the services. Patients typically pay through checks or credit cards (via patient portals) and these need to be correctly accounted against the claim to avoid any inflated AR and proper closing of the claim.
Denial Management
Operomed, is dedicated to minimize lost reimbursements and denials with highly efficient systems and services designed to meet our clients’ needs. One of the major problems faced by healthcare providers and medical billing companies is that a large proportion of rejected claims goes unattended and is never resubmitted. Our Denial Management process uncovers and resolves the problem leading to denials and shorten the accounts receivables cycle. The denial management team establishes a trend between individual payer codes and common denial reason codes. This trend tracking helps to reveal billing, registration and medical coding process weaknesses that are then corrected to reduce future denials, thus ensuring first submission acceptance of claims. Also, the payment patterns from various payers are analyzed for setting up a mechanism to alert when a deviation from the normal trend is seen.
Accounts Receivable Management
At Operomed, the AR management team is structured to be a complete solution provider to address difficulties that occur in cash flows and is operated as a part of the medical billing team. The goal here is to recover the funds owed to the client as quickly as possible. We aim at accelerating cash flows and reducing the Accounts Receivable days by submitting error free clean-claims, proper analysis of denied claims and regular follow-ups with insurance companies and patients for outstanding claims and dues.